Sleep Apnea and Glaucoma
This post was originally posted on September 10, 2013, and updated on July 15, 2022.
With a significant percentage of Obstructive Sleep Apnea (OSA) patients suffering from some forms of glaucoma, researchers have begun to study the relationships between the two conditions over the last several years. For OSA patients that are also living with glaucoma, the questions regarding the effects of CPAP therapy via a CPAP machine are real and ongoing.
What is Glaucoma?
Glaucoma is actually composed of several optic nerve-damaging eye conditions. It is typically caused by high pressure within the eye, according to the Mayo Clinic. Symptoms are usually slow-progressing, with vision loss being one of the only signs. Some of the glaucoma risk factors such as age are very common while others such as ethnicity are less so.
A number of clinical studies over the last several years have shown an association between sleep apnea and several glaucoma indicators. This includes intraocular pressure (IOP), visual field means deviation, cup-to-disk ratios, and retinal nerve fiber layer thickness. More recently Taipei Medical University researchers published results from a study in the journal, Ophthalmology. It showed OSA patients have a higher risk of developing glaucoma compared with people without the sleep disorder.
There are many studies showing the reduction in IOP among glaucoma patients following the use of a CPAP machine. Still, the complexities of glaucoma as well as the wide variations in OSA severities make a direct correlation more elusive. Some studies have suggested that CPAP therapy can even raise IOP to some degree. But, many researchers generally agree that the risk is possible in a smaller subset of OSA patients.
Even then, most researchers and medical experts see the increased oxygen levels attained through the use of a CPAP machine and the overall health benefits far outweighing the hypothetical risks. The takeaway for OSA patients, especially those with severe forms of the condition, is to work with their physician and sleep therapist to monitor all physiological conditions and ask questions.
The direct links between increased risk of hypertension, high blood pressure, obesity, OSA, and other severe health risks are becoming clearer each day. Some still see the effects of sleep apnea on ocular blood flow as being in the hypothetical phase. But, there are several current studies looking at sleep and IOP. In fact, the Mayo Clinic has many Glaucoma research studies focusing on circadian changes and how sleep can impact glaucoma.
Obstructive sleep apnea leads to decreased oxygen levels in the blood, known as hypoxia. There is evidence that hypoxia in these patients results in a number of changes that may ultimately affect the blood flow to the optic nerve.
In addition, obstructive sleep apnea leads to fluctuations in blood pressure that may alter the balance between blood pressure and pressure in the eyeball, leading to less blood flow to the eyeball. The reduced blood flow to the optic nerve increases the risk for optic nerve damage. Along with other known risk factors for glaucoma — such as family history, age, diabetes, myopia and thin corneas — obstructive sleep apnea can increase a person’s susceptibility to glaucoma.
According to their research, Intraocular pressure (IOP) varies throughout the day with the highest pressures occurring during sleep. While these changes happen for everyone regardless of health, the reasons are still unclear.
What we do know, and what is becoming even clearer, is that sleep has a profound effect on our health. With the proven benefits for millions of OSA patients using a CPAP machine, more restful sleep lead to healthier lives.
Best Sleeping Position for Glaucoma
Doctors know intraocular pressure (IOP) rises at night and when the patient is in the supine position. To mitigate the effect on patients with glaucoma, and those at-risk, some doctors have proposed glaucoma patients sleep sitting upright. Reducing pressure on the eye may require using pillows to prop yourself up, even though it may not be as comfortable.
Wedge pillows are another option for glaucoma patients that can help keep the head elevated and reduce eye pressure while still providing some comfort while sleeping. Sleeping on a wedge-shaped pillow that elevates the head 20 degrees reduces nighttime intraocular pressure (IOP) and thereby might help control or reduce the risk of glaucoma.
Sleeping Posting That Can Worsen Glaucoma
In comparison to sleeping upright, one study found that people with worsening glaucoma on just one side were also more likely to sleep with the affected eye facing downward. The researchers say that position raises the eye's internal pressure and probably hastens deterioration of the eye.
Side sleeping and stomach sleeping were some of the worst positions a person with glaucoma can take. Extra pressure was applied to the eye during these positions. Sleeping on the back also applies pressure almost equally to other positions.
Glaucoma patients have little choice but to find a way to sleep comfortably while applying zero pressure on the eyes, which means sleeping upright.
Effect Of Different Sleeping Positions for Glaucoma Patients
Glaucoma patients can do many things to help manage their eye disease. Patients can follow a regiment of medications and look to proper diet. Sleep position is also an important factor for glaucoma patients.
When glaucoma patients slept on their back, side or stomach, pressure increased on the eye. This applied pressure, due mainly to gravity, lasted up to eight hours while glaucoma patients slept. This further increased damage to the eye long-term, including leading to blindness.
Glaucoma patients must look to other sleeping positions that reduce eye pressure. This could be sleeping upright or with a wedge pillow that keeps the head elevated enough to reduce pressure.
For additional information on various topics concerning sleep apnea and CPAP products, please refer to our blog. It has updates and offers free advice and information. If you’d like to learn more about the quality sleep apnea products we carry, call us at (866) 414-9700. You can also contact us through our website, or add our app for additional discounts. https://www.thecpapshop.com/contact-us
Key Takeaways
- Glaucoma is typically caused by pressure within your eye and can result in vision loss if not properly treated.
- While there is no direct connection, having sleep apnea increases the risk of someone also developing glaucoma.
- Getting the proper amount of sleep every night has proven to have a significant impact on a person's overall health and wellness.
With a significant percentage of Obstructive Sleep Apnea (OSA) patients suffering from some form of glaucoma, researchers have begun to study the relationships between the two conditions over the last several years. For OSA patients who are also living with glaucoma, the questions regarding the effects of CPAP therapy via a CPAP machine are real and ongoing.
What is Glaucoma?
Glaucoma is actually composed of several optic nerve-damaging eye conditions. It is typically caused by high pressure within the eye, according to the Mayo Clinic. Symptoms are usually slow-progressing, with vision loss being one of the only signs. Some of the glaucoma risk factors such as age are very common while others such as ethnicity are less so.
Connection Between Sleep Apnea and Glaucoma
A number of clinical studies over the last several years have shown an association between sleep apnea and several glaucoma indicators. This includes intraocular pressure (IOP), visual field means deviation, cup-to-disk ratios, and retinal nerve fiber layer thickness. More recently Taipei Medical University researchers published results from a study in the journal, Ophthalmology. It showed OSA patients have a higher risk of developing glaucoma compared with people without the sleep disorder.
There are many studies showing the reduction in IOP among glaucoma patients following the use of a CPAP machine. Still, the complexities of glaucoma as well as the wide variations in OSA severities make a direct correlation more elusive. Some studies have suggested that CPAP therapy can even raise IOP to some degree. But, many researchers generally agree that the risk is possible in a smaller subset of OSA patients.
Even then, most researchers and medical experts see the increased oxygen levels attained through the use of a CPAP machine and the overall health benefits far outweighing the hypothetical risks. The takeaway for OSA patients, especially those with severe forms of the condition, is to work with their physician and sleep therapist to monitor all physiological conditions and ask questions.
Does Sleep Apnea Cause Glaucoma?
Although the two diseases are not directly related, some studies do show that sleep apnea patients are more likely to develop glaucoma than those who do not have sleep apnea. Sleep apnea can cause pressure on the eyes, so it is always recommended to see an eye doctor, especially if you have sleep apnea.
Additionally, undiagnosed and untreated sleep apnea could lead to worse problems for your eyes. Not treating sleep apnea can have numerous effects on the body, including ocular pressure, which could lead to more severe problems, like blindness, over time.
What is the First Sign of Glaucoma?
The first sign of glaucoma typically is the loss of vision on the sides of your eyes. Additionally, some people may start to see rings or "halos" around lights or see rainbow-colored cicles around lights. You may also become more sensitive to light. If you are experiencing any of these symtpoms, it is crucial you go see your eye doctor.
What Consequences Does Sleep Apnea May Have On Your Eyes?
The direct links between increased risk of hypertension, high blood pressure, obesity, OSA, and other severe health risks are becoming clearer each day. Some still see the effects of sleep apnea on ocular blood flow as being in the hypothetical phase. But, there are several current studies looking at sleep and IOP. In fact, the Mayo Clinic has many Glaucoma research studies focusing on circadian changes and how sleep can impact glaucoma.
Obstructive sleep apnea leads to decreased oxygen levels in the blood, known as hypoxia. There is evidence that hypoxia in these patients results in a number of changes that may ultimately affect the blood flow to the optic nerve.
In addition, obstructive sleep apnea leads to fluctuations in blood pressure that may alter the balance between blood pressure and pressure in the eyeball, leading to less blood flow to the eyeball. The reduced blood flow to the optic nerve increases the risk of optic nerve damage. Along with other known risk factors for glaucoma — such as family history, age, diabetes, myopia, and thin corneas — obstructive sleep apnea can increase a person’s susceptibility to glaucoma.
How To Reduce The Risk Of Glaucoma And OSA?
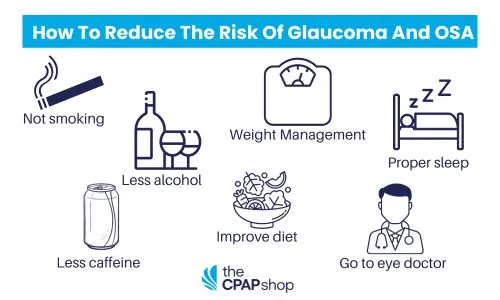
There are several steps you can take to lower your risk of developing sleep apnea and glaucoma. They include:
- Not smoking
- Drinking less alcohol
- Drinking less caffeine
- Improving your diet
- Proper weight management
- Getting an adequate amount of sleep
- Regularly seeing your eye doctor and taking any medications as prescribed
Best Sleeping Position for Glaucoma
Doctors know intraocular pressure (IOP) rises at night and when the patient is in the supine position. To mitigate the effect on patients with glaucoma, and those at-risk, some doctors have proposed glaucoma patients sleep sitting upright. Reducing pressure on the eye may require using pillows to prop yourself up, even though it may not be as comfortable.
Wedge pillows are another option for glaucoma patients that can help keep the head elevated and reduce eye pressure while still providing some comfort while sleeping. Sleeping on a wedge-shaped pillow that elevates the head 20 degrees reduces nighttime intraocular pressure (IOP) and thereby might help control or reduce the risk of glaucoma.
Sleeping Posting that Can Worsen Glaucoma
In comparison to sleeping upright, one study found that people with worsening glaucoma on just one side were also more likely to sleep with the affected eye facing downward. The researchers say that position raises the eye's internal pressure and probably hastens the deterioration of the eye.
Side sleeping and stomach sleeping were some of the worst positions a person with glaucoma can take. Extra pressure was applied to the eye during these positions. Sleeping on the back also applies pressure almost equally to other positions.
Glaucoma patients have little choice but to find a way to sleep comfortably while applying zero pressure on the eyes, which means sleeping upright.
Effect Of Different Sleeping Positions for Glaucoma Patients
Glaucoma patients can do many things to help manage their eye disease. Patients can follow a regiment of medications and look to a proper diet. Sleep position is also an important factor for glaucoma patients.
When glaucoma patients sleept on their back, side, or stomach, pressure increasesd on the eye. This applied pressure, due mainly to gravity, lasted up to eight hours while glaucoma patients slept. This further increased damage to the eye long-term, including leading to blindness.
Glaucoma patients must look to other sleeping positions that reduce eye pressure. This could be sleeping upright or with a wedge pillow that keeps the head elevated enough to reduce pressure.
Facts about Glaucoma
- 3 million Americans suffer from glaucoma, which is the second most common cause of blindness globally.
- A large number of glaucoma patients are still undiagnosed.
- Globally, there were around 80 million cases of glaucoma in 2020; by 2040, that number is predicted to rise to nearly 111 million.
- Glaucoma damages the eye’s optic nerve.
- Once glaucoma damages your optic nerve, lost vision cannot be restored.
- There are 25 million Americans and 100 million people worldwide who suffer from sleep apnea.
- Because breathing can cease for up to two minutes, a blocked airway might result in snoring, gasping, or choking.
Concluding Thoughts on Sleep Apnea and Glaucoma
According to their research, Intraocular pressure (IOP) varies throughout the day with the highest pressures occurring during sleep. While these changes happen for everyone regardless of health, the reasons are still unclear.
What we do know, and what is becoming even clearer, is that sleep has a profound effect on our health. With the proven benefits for millions of OSA patients using a CPAP machine, more restful sleep leads to healthier lives.
For additional information on various topics concerning sleep apnea and CPAP products, please refer to our blog. It has updates and offers free advice and information. If you’d like to learn more about the quality sleep apnea products we carry, call us at (866) 414-9700. You can also contact us through our website.









