Talking CPAP with Sleep Therapist Dr. Indira Gurubhagavatula
The CPAP Shop recently attended the 7th annual Philadelphia Sleep Conference, a one-day intensive continuing education seminar for sleep specialists. Dr. Indira Gurubhagavatula, associate professor of medicine at the Veteran’s Administration Medical Center at the University of Pennsylvania, served as a presenting faculty member. A graduate of John Hopkins University School of Medicine and Harvard School of Public Health, Dr. Gurubhagavatula focuses her research and work on the screening of obstructive sleep apnea, sleep-disordered breathing and cardiovascular disease, and sleep disorders medicine, including CPAP therapy.
Chris Vasta of The CPAP Shop spoke with Dr. Indira Gurubhagavatula on the impact of CPAP therapy on sleep apnea.
Sleep apnea is undertreated for a variety of reasons. The first is under diagnosis. Secondly, some patients lack the supports to help them find the treatment that works best for them, and later, to help them in adjusting and adapting to that therapy. For example, adjusting to CPAP may be difficult. If so, the right supports can make a huge difference in helping the patient receive effective therapy, and in return, getting the many benefits of this therapy.

The Diagnosis Challenge
Q. Why is sleep apnea underdiagnosed and undertreated—and what are the implications of that?
Dr. Gurubhagavatula: Sleep apnea is sometimes missed because people are unaware that they even have the classic symptoms of the disorder. Also, some patients may be reluctant to report symptoms because they are self-conscious or embarrassed, or out of fear of being labeled lazy.
These symptoms happen when the individual is sleeping and may include snoring, choking or gasping during sleep. Often times, the person may not be aware of this even happening. In fact, the reason that symptoms like this come to attention is that the snoring is so loud that it bothers other people. Or, the person experiences sleepiness during the day after repeatedly having to wake up to take a breath during sleep.
Many times, especially if the person does not have a bed partner and no one has observed them sleeping, they may not find out for many years that they have the condition. Further, additional barriers to diagnosis include lack of access to health insurance or healthcare providers not thinking about it and making the appropriate referrals to get the testing done. Sleep apnea tends to be increasingly underdiagnosed in women.
Upon diagnosis, the first-line treatment for sleep apnea is continuous positive airway pressure (CPAP). Other options may include wearing an appliance in the mouth during sleep or having surgery.
Screenings and Indicators for Sleep Disorders
Q. How do you screen for sleep apnea? Are there particular indicators that you look for?
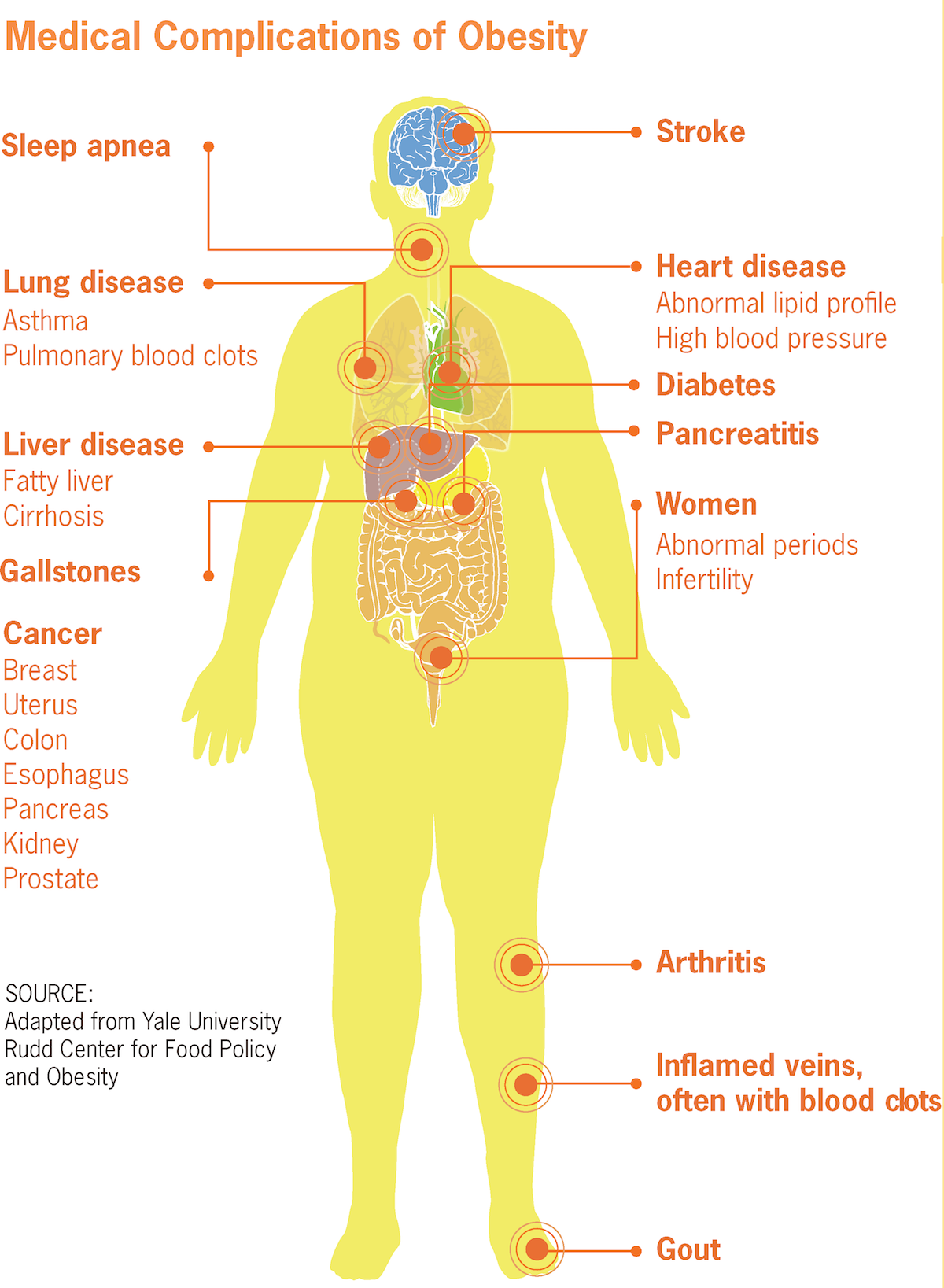
Dr. Gurubhagavatula: The major risk factor for sleep apnea is obesity. Screening may also include an assessment for common symptoms, like snoring, daytime sleepiness, or a family history of the disorder. Another condition that increases the risk for sleep apnea includes low thyroid function.
Impact of CPAP Therapy
Q. How do you recommend treating sleep apnea?
The first-line treatment is CPAP therapy. This is recommended first for patients with moderate to severe sleep apnea. For milder cases, other options, such as an oral appliance or surgery, may be considered. Along with these treatments, patients should lose weight to fall into a healthy range.
In addition, the treatment also includes keeping any nasal congestion well-controlled and limiting the use of alcohol and any medications that may worsen daytime sleepiness.
Q. When it comes to weight loss (or any other alternative) versus CPAP therapy, what does your research indicate? How does each intervention work independently and in conjunction with one another?
Dr. Gurubhagavatula: CPAP therapy is backed by the greatest volume of scientific evidence for the treatment of sleep apnea. In obese patients with sleep apnea, weight loss has many general health benefits, such as lowering the risk of cardiovascular disease. Weight loss may improve sleep apnea in some individuals but is difficult to achieve for long periods of time. Many people regain the weight they lose. Large amounts of sustained weight loss, such as the kind that occurs after weight loss surgery in very obese individuals, may resolve sleep apnea in some (but not all) patients.
We generally recommend that people who use CPAP therapy for their sleep apnea should also attempt to lose weight. Collectively, the two treatments give patients a greater chance of improving the inflammation that contributes to cardiovascular disease.
Long-Term Success with CPAP
Q. What are the benefits of CPAP therapy and why is it important?
Dr. Gurubhagavatula: CPAP can correct oxygen levels, eliminate snoring and improve the quality of sleep. Additionally, CPAP also improves sleepiness, blood pressure control, headaches, mood, memory, and the ability to sustain attention. Finally, CPAP reduces the risk of sleepiness-related vehicle crashes in drivers.
Q. Once CPAP therapy begins, how do achieve long-term adherence? Do you have any tips for success?
Dr. Gurubhagavatula: Once CPAP treatment begins, close follow-up is needed—especially in the initial days and weeks. Patients who do not use CPAP long-term tend to establish this pattern of non-use quite early.
Supportive interventions should be available at the onset of therapy. This includes a foundation of strong education about sleep apnea, its risk and consequences, and the benefits of CPAP therapy. The CPAP mask should be well-fitted and comfortable. Specific treatments are available for patients with claustrophobia, to help them overcome this issue.
Any nasal congestion should be well-controlled. The bedroom environment should be quiet, dark, cool and comfortable. Patients should maintain good sleep hygiene—i.e., habits that promote sound sleep. This means limiting caffeine and alcohol, getting adequate exercise, and choosing healthy foods. Treatment for any co-existing general medical or sleep disorders should be optimized so that the patient has the best chance of success with CPAP therapy.
If you have questions about starting CPAP therapy or need help picking the right products to fit your needs, give us a call at The CPAP Shop.
[magento store="1" sku="DSG500S11-BUNDLE, DSX500S11-BUNDLE, 37207-BUNDLE, 38113-BUNDLE" order="sku" dir="desc" limit="4" class="override"]




